I’m just bringing a snapshot of ours next week just in case. But I will leave the actual cards at home.
I understand and I appreciate the info in this thread too b/c I’m worried at some point that my CDC card won’t be good enough or if they are lost. I’m afraid of carrying them around even though I’ve laminated them  . I know my dr. has record of my shots, dates, type etc. DH’s vaccinations are recorded w/ the DoD/VA.
. I know my dr. has record of my shots, dates, type etc. DH’s vaccinations are recorded w/ the DoD/VA.
I thought about that, but was concerned about them being able to easily add shot #3 info. (Or in my J&J case, #2 ![]() )
)
We are getting by with 3 pair of uniform shorts and 3 uniform shirts for now. Laundry all.the.time. The school has informed us that they will suspend the “must by pants from” rule, and allow us to purchase navy slacks from Old Navy if we need them in an emergency.
School gave us all plastic sleeves. One side is colored with our district logo, the other side clear.
I do not want to take them to FL- too much water/rain
I bought plastic sleeves off of Amazon for ours.
For WDW/UOR I wouldn’t worry about taking a vaccine card. Now if you are going to California, that’s a different story. Universal will be requiring them starting in a few weeks since they are in LA County and that is their new rule. It remains to be seen if DLR will follow suit since they are in Orange County.
At the time shot #3 wasn’t a thing… oh well.
I’ve lost track of the responses to this topic of school uniforms, but I wanted to report that as soon as I asked about a waiver for my son’s pants it was granted. Ok to wear same color ones without the special logo until Flynn O’Hara ones come in. Very relieved! This school is known for being very strict about its uniforms but this is a really unusual time and I’m glad they are being reasonable. They do have a used uniform organization, but were sold out of his size when I checked.
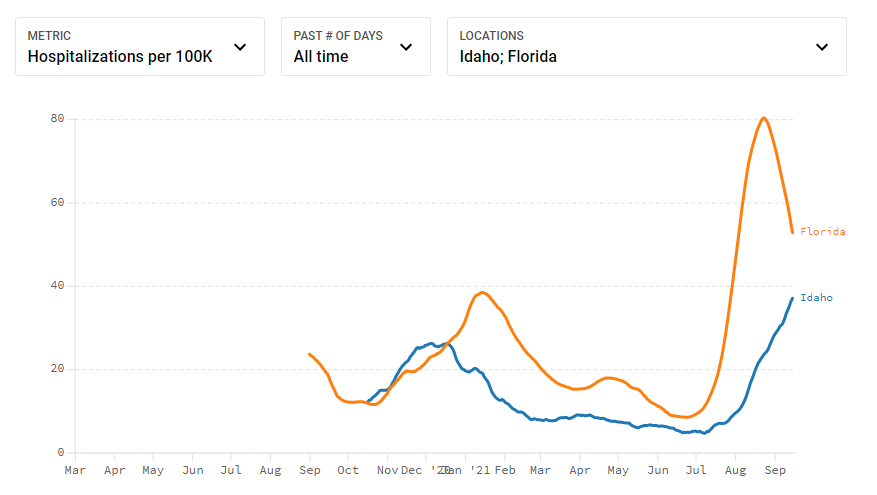
One place that is not doing so great right now is Idaho. My sister shared this article about how hospital emergency rooms are now implementing “crisis standards” - i.e., they won’t provide the same level of care as usual since there’s no capacity.
Hospitalizations are still on the upsurge - rising to meet Florida’s retreat, even though Idaho has a younger population and therefore not as much existing hospital capacity.
That’s not good news.
Yep, Idaho is our neighbor and we have a lot of their patients over here in Spokane. They still refuse masking and vaccinating, so this will continue until it burns through everyone I guess. Sigh.
This was on the news last night, this is where I work (not in the ICU thankfully).
There are still questions about covid reporting in FL by state officials.
COVID-19 deaths continue at Florida prisons, though agency no longer reports them - Orlando Sentinel At least two men recently died of COVID-19 while serving prison sentences in Florida, the Orlando Sentinel confirmed through medical examiners, though the state department of corrections has stopped reporting such deaths, or even cases, publicly.
The deaths raise further concern about the ongoing — and unknown — threat of COVID-19 in state correctional facilities, for both the incarcerated and staff. Since early June, when the Florida Department of Corrections halted emergency pandemic protocols, including all reports on COVID-19 cases, testing and deaths, it’s been unclear the extent of the virus inside state prisons without accurate or up-to-date data. Advocates and families continue to hear frequent reports of COVID-19 symptoms and a lack of testing inside many prisons.
FDC officials did not respond to questions this week from the Sentinel about an updated count of COVID deaths among incarcerated people, or if the agency is reconsidering its plan to no longer update a COVID dashboard. FDC officials also did not provide current positive case numbers among the more than 80,000 people in Florida prisons.
“It’s tough to sit with the fact that some of these most basic, foundational concerns aren’t really being answered,” said Forrest Behne, the policy director for the COVID Prison Project, which tracks the virus at correctional facilities nationwide. “We would love to be able to advise on practices that are informed by that data, but that’s not possible.”
COVID-19 kills over 50,000 in Florida - Orlando Sentinel
During the COVID-19 delta variant surge, morgues overflowed into mobile units. Crematories got backlogged. Funeral homes were deluged with calls. Under-staffed shifts and dangerous working conditions tested the hospital workers who hadn’t already quit.
Now, as the fourth wave ends, Florida has reached 50,000 COVID-19 deaths. Thursday’s grisly milestone comes from data reported to the U.S. Centers for Disease Control and Prevention by the Florida Department of Health. Over 666,000 have died nationwide.
In Central Florida’s most populous county, Orange, 337 people died from COVID-19 throughout August, the deadliest month of the pandemic. That number, about a fifth of the county’s 1,780 COVID-19 deaths, is accurate as of Monday, according to Dr. Raul Pino, county DOH director. The toll may rise as more deaths are confirmed.
This fourth wave was initially predicted to cause fewer deaths and hospitalizations than past waves due to the widespread availability of free vaccines. But when the first shots were given on Dec. 14, the state’s death count was 21,410. That means that nearly 30,000 deaths have been reported in the interim, more than half of the pandemic’s total.
“There is no question that the delta variant had changed everything,” Pino said when asked about the month’s record-breaking deaths at an Aug. 27 news conference. “But if we were at higher rates of vaccination, let’s say 80 to 85% of our eligible population, the numbers would be smaller.”
Statewide, 13,281,666 residents, or 69% of people age 12 and up, have received at least one vaccination shot, including 11,048,444 who have completed their shot regimens through Sept. 9.
Since vaccines have become available, Central Florida hospitals have consistently reported that the vast majority of those who have gotten seriously ill and died have been unvaccinated — typically, over 90%.
In recent days, Gov. Ron DeSantis has continued to fight mask and vaccine mandates from schools and private companies, and has threatened local governments with millions of dollars of fines.
Asked about the 50,000 deaths at a news conference in Fort Lauderdale on Thursday, he said, “I think it’s been a really tough year and a half … I think it’s been really, really rough.”
DeSantis, one of several leaders who seemingly underestimated the delta variant, went on to say that his efforts to promote the Regeneron antibody treatment for those infected with COVID-19 had helped to “mitigate that” death count and would continue to do so.
Health experts say it is difficult to assess whether that claim is true without detailed studies, but anecdotal evidence from doctors and patients suggests it has kept high-risk people from getting severely ill.
It’s worth noting that there’s debate over when this milestone really happened. The Institute for Health Metrics and Evaluation suggests that the state actually hit the 50,000 mark in early May.
But the specifics don’t change the fact that thousands of Central Florida residents have been lost to COVID.
As the numbers inched closer to this landmark total, Orange County Mayor Jerry Demings wondered if anyone noticed that 50,000 Florida residents had succumbed to the virus.
“I’ve been to funerals or viewings each week lately between … my employees, my classmates and friends who have been dying left or right,” said Demings last week. “It’s almost like an afterthought now, almost like nobody cares that 50,000 people have died from the coronavirus here in the state of Florida.”
Fatigue, trouble breathing, pain:
1 in 3 COVID-19 patients suffer from long COVID, CDC finds
Rong-Gong Lin II and Luke Money,
Los Angeles Times
LOS ANGELES — A new study has found that 1 in 3 people who survived COVID-19 suffer from long COVID.
The study of Long Beach residents published by the U.S. Centers for Disease Control and Prevention on Thursday found that these long COVID patients reported at least one symptom of COVID-19 two months after first testing positive for the coronavirus.
There were higher rates of long COVID among people 40 or older, women, people with preexisting health conditions and Black residents, according to the study, conducted by the University of California, Davis epidemiologists and the Long Beach Department of Health and Human Services.
The survey was based on the responses of 366 adults in Long Beach who tested positive for the virus last year, before vaccinations were authorized for emergency use and began to be rolled out to health care workers.
The study found that 35% of survey responders reported at least one ongoing symptom of COVID-19 two months after the initial positive test.
Fatigue was reported by 17% of those long COVID patients; difficulty breathing and loss of taste or smell were reported by 13%; and muscle or joint pain was reported by 11%.
The study authors said the results are important to help experts “develop efforts to prioritize prevention and treatment strategies for” populations at higher risk of long COVID.
The study’s results are limited by the relatively small number of people surveyed, and it wasn’t possible to attribute symptoms to COVID-19 versus those that existed before coronavirus infection. It’s also possible that people with long COVID symptoms were more likely to respond to the survey, according to the report, meaning the study might potentially overstate the problem.
“Further research, including research over longer periods, is warranted,” the study said.
The study was published in the CDC’s Morbidity and Mortality Weekly Report.
Experts say that vaccination not only reduces the chance of falling ill with COVID-19, but also probably reduces the chance of enduring long COVID should a vaccinated person contract a breakthrough infection.
Vaccinated people are far less likely to be infected or get severely ill from COVID-19 than unvaccinated people.
“If the virus can’t take hold in your body — if it can’t get into your system and if it can’t start replicating — then it doesn’t have a chance to get to the point where you might translate into having long-haul symptoms,” Dr. Christina Ghaly, the L.A. County director of health services, said this year.
©2021 Los Angeles Times. Visit at latimes.com . Distributed by Tribune Content Agency, LLC.
1 in 3 seems like an awful lot. I think the UK study found it was 5%.
Yes, I was just reading about that today… Link.
Thank you so much for sharing that. I’m shocked but glad that the ICU was willing to let reporters in to do a story.
I think it depends on your definition of long Covid. This study looked at 2 months or longer. So it includes people who have symptoms for 2-3 months. The UK study looks at longer than 12 weeks.
LOL… I read the symptoms in this link and they are the same symptoms for my thyroid disease